By Angie Comfort, RHIA, CDIP, CCS, CCS-P
The arrival of October 1, 2015 was met with anxiety, alarm, and even terror by many as the healthcare industry braced for what some called “another Y2K-like event”—the ICD-10-CM/PCS implementation. Fast-forward to September 2017, where we have been living in the post-ICD-10 world for almost two years. While there have definitely been trials, there have also been many triumphs.
Decreases in Productivity
It’s possible that we all know at least one person in the industry that would make “the sky is falling” exclamations whenever the subject of productivity came up with ICD-10-CM/PCS. But in reality, the decrease of productivity for prepared outpatient and physician encounters only lasted for a few months following implementation—if there was much of a decrease at all. Facilities and physician practices that invested the time in training their staff on ICD-10-CM and developing new—or adjusting old—processes seem to have weathered the storm better than those that carried on believing and operating as though the implementation would never happen.
While providers that were prepared did experience a decrease in productivity, that decrease was a drop in the proverbial bucket compared to the decreases experienced by those that were not prepared. By having to take the extra time to get their staff trained on the new system that was implemented without another delay, these facilities and practices saw a greater decrease in their productivity. They had to hurriedly educate their staff and update their processes right before the ICD-10 implementation—in some cases, this even took place after ICD-10-CM was implemented. These delays resulted in a drastic decrease in productivity, which in turn led to a decrease in cash flow.
On the flip side is the ICD-10-PCS code set, which is still causing angst for inpatient coding professionals and their managers. The productivity decrease is very apparent here. Some procedures that only required one procedure code under ICD-9-CM now require several ICD-10-PCS codes to tell the story of the procedure performed. This has been the major area of concern for even seasoned coding professionals, as they are seeing a large decline in their coding productivity.
This is a challenge that will continue. Lack of education and preparation is not the issue for coding professionals in this area; they are simply dealing with an influx in the number of codes required to completely describe the procedures they are coding.
Increases in Staffing
While the majority of practices and healthcare organizations did not feel the need to hire additional coding professionals as employees, a lot of them did hire consulting companies to help during the transition. Several consulting firms acknowledged that they were at full capacity during the months leading up to and following the ICD-10 implementation. While the facilities themselves did not hire employees, these consulting firms did. Some companies even offered huge incentives such as cash sign-on bonuses or the opportunity to win a car to entice coding professionals knowledgeable in ICD-10 coding to come join their teams. The demand for consulting is not currently at the all-time high it was during ICD-10 implementation, but it is still a much needed service in some facilities, such as quality audits of the ICD-10 code set. These companies not only offer interim coding staff support, they also offer external audits and education directly to a facility’s employees.
Left, Right, Unknown
Documentation issues have been at the forefront of the trials of ICD-10 implementation. For years (due to all the delays), most facilities and physician practices were already prepping their physicians to improve their documentation for the specificity of ICD-10. This greatly assisted those organizations in being prepared for the increased amount of queries—and even curtailed much of the need for queries based on their physician education that had taken place during the transition period. One facility said they did not even tell the physicians that their new clinical documentation improvement (CDI) program was for ICD-10 because the delay pushed the implementation back another year and they wanted their providers to be completely ready for go-live.
In a February 2017 ICD-10 Watch blog post, Carl Natale explained that when physicians are complaining about ICD-10, it is usually related to the documentation aspect of the coding system.1 “ICD-10 compliance becomes a much smaller problem after clinical documentation improvement,” Natale says. There is great truth in this statement. Compliance with ICD-10 is an easier problem to deal with when you have a good CDI program.
Examining Claims Denials
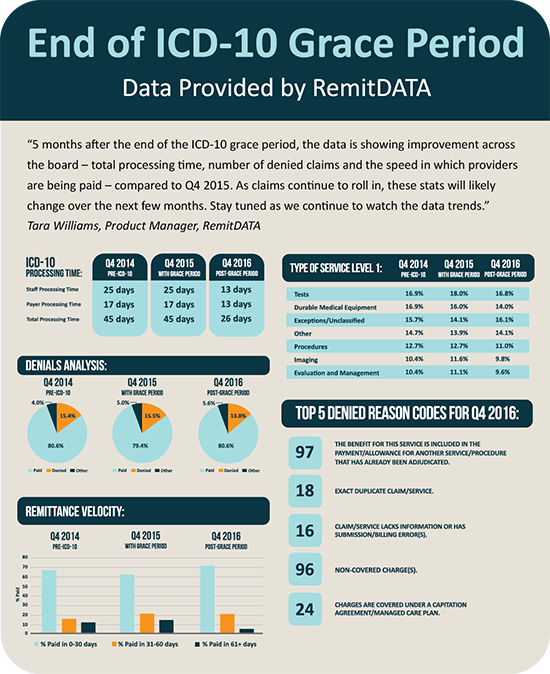
In October 2016, the grace period for ICD-10 flexibilities for providers expired. This grace period allowed providers to submit unspecified codes in a code family to Medicare for claims processing while giving the providers another year to ramp up their documentation for the increased specificity. Did the additional year of safe harbor really help the providers? The Centers for Medicare and Medicaid Services (CMS) created an ICD-10 Next Steps Toolkit for providers, which assisted them in using key performance indicators (KPI) to identify issues with reimbursement, claims processing, and other areas.2 A few of these include days to final bill, days to payment, claims acceptance/rejection rates, and claims denial rates. By using a tool such as this, the providers are able to quickly determine if they are having issues with their claims.
Remitdata.com created an infographic, originally published in Physicians Practice, that shows some very interesting data on provider claims (see the sidebar above). According to their study, “things are going well” with ICD-10. By reviewing their data, it shows that the total days of processing a claim has been cut almost in half with ICD-10 and claim denials are back to the same percentage before ICD-10 implementation. This study agrees with the discussion in Sue Bowman’s Journal of AHIMA article “Look Back on the ICD-10 Transition: Crisis Averted or Imaginary?”3 There was not a huge increase in denials or rejected claims after the transition. In fact, Bowman states that “for the most part, the claims have been successfully submitted and processed.”
Looking Ahead
The common thread seen in the success of the ICD-10 implementation is the great lengths that those who prepared went to in order to educate and train not only their coding professionals, but their entire facility or practice. The implementation of ICD-10 affected every aspect of an organization. Those who made the effort to be prepared for this momentous change were able to see the benefit of their efforts.